Benefits of Bariatric Surgery: Bariatric surgery has been around for a long time; well over 60 years. Originally, it was considered experimental, dangerous, fringe medicine but it is now known to be safe, routine, elective, and the standard of care.
The concept of a “simple” weight-loss surgery is outdated as it is now seen as a life-changing metabolic surgery.
This means these surgeries have positive, beneficial effects on other medical conditions, such as diabetes, high blood pressure, and obstructive sleep apnea. These, along with a whole host of other diseases, have only been controlled or managed, rather than cured.
Bariatric surgery patients get off their diabetes medicines quickly – sometimes the day of surgery. Their blood pressure medication requirements go down with weight loss. Their acid reflux is improved and/or cured, their cholesterol normalizes, and they get off their CPAP machines. Their arthritis improves, their hearts and lungs no longer work as hard, and their quality of life improves.
Bariatric surgery is not for everyone, but if your BMI is over 40, and you have any of the conditions listed above, your life could be changed forever.
What to Expect: There is a process that every patient follows for bariatric surgery. The process begins with the patient attempting to lose weight by other means, as counseled by his/her doctor. If this plan fails, then bariatric surgery is considered.
All patients go through several months of preoperative classes and training. This includes visits with the surgeon, nursing staff, bariatric dietitians, and trained psychologists. This is dictated by the patient’s insurance company but much of it is also common sense.
All patients are expected to lose weight during the process. Ten percent (10%) of their starting weight is a good goal. Each patient will also get medical clearance appropriate to their health.
Once the insurance approval process is completed, surgery is scheduled. For two weeks prior to surgery, patients will be on a liquid diet. The liquid diet will be continued for four (4) weeks after surgery. It is anticipated that the patient will be hospitalized for only one day with an overnight stay.
Patients will be walking within hours, sipping on ice chips. The next morning, the liquid diet will be resumed, which consists of protein shakes and water.
Patients will be discharged later that afternoon, and their first follow-up visit will be 7 – 10 days later. Follow-up visits will continue at 4 weeks, 6 weeks, 3 months, 6 months, then yearly.
Patients will be encouraged to eat well, exercise regularly, take their vitamins properly, and continue to follow-up long term.
Life after Surgery: Life after bariatric surgery is not easy but well worth it.
The first few weeks of surgery, patients are adjusting to their new stomach anatomy and have to remain on a carefully controlled liquid diet.
Their activity quickly advances back to normal. They may take a week or two off from work, but there is very minimal pain after a few days and there are no restrictions in activity for the motivated patient.
After a few weeks, we advance the diet to soft foods, including things like tuna salad, egg salad, lunch meat, eggs, cheese, and yogurt. Then, over the next few months, we advance to normal foods – mostly meat, a little bit of cooked vegetables, and very little else,
Patients are encouraged exercise and are reminded eat their small meals slowly and regularly, even if they are not hungry, and minimize snacking.
Patients who follow these practices faithfully will lose about two-thirds (2/3) to three-quarters (3/4) of their excess weight in the first year after surgery.
Along with this weight loss comes resolution of other medical conditions, such as diabetes, hypertension, acid reflux, and obstructive sleep apnea.
Quality of life improves, and patient satisfaction is excellent.
Types of Bariatric Surgery
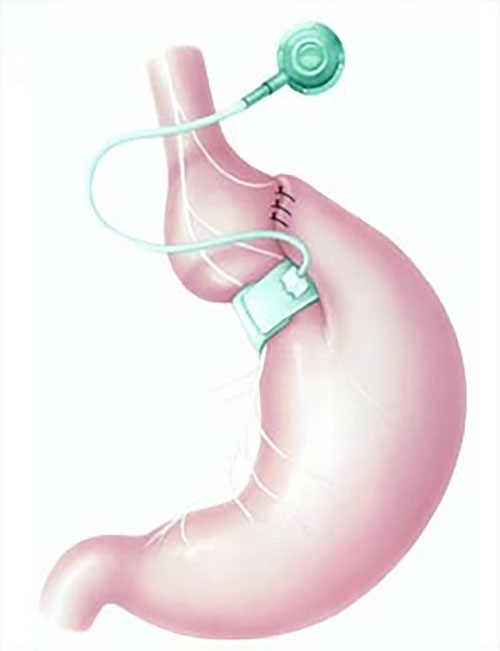
Gastric Band:
Gastric Banding has been around for a long time and has gone through many revisions over the years.
The surgery is performed laparoscopically. A small device is placed in the abdomen and wrapped around the top of the stomach. It is stitched into place and connected to a tube, which is connected to a port. The port is sutured to the abdominal muscles, under the skin, and accessed with a needle. Small injections of saline, made over time, can tighten or loosen the band.
The intended effect is to provide patients with a sense of satiety (satisfaction or a feeling of being full) when eating small meals. If patients eat small meals consistently, along with progressive exercise, they will slowly lose weight over time.
The band does not restrict patients from eating larger meals or snacking slowly throughout the day, however, and it does not help patients choose their foods wisely. It takes extreme motivation and discipline to make the band work.
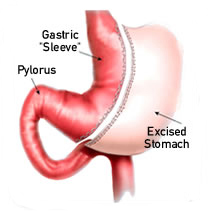
Gastric Sleeve:
The Vertical Sleeve Gastrectomy, or Gastric Sleeve, is a new procedure that has gained popularity. Also a laparoscopic surgery, it is probably the most commonly performed operation today.
During this surgery, the stomach is divided with staplers in a vertical (up and down) fashion to create a tube-shaped organ. The pressure in the tube is fairly high, causing food to move through it quickly. The remainder of the stomach is removed through one of the small incisions in the abdomen. The incisions are closed, and the operation is complete. There are no devices to manage and no bowel connections to be made.
The operation is relatively simple, and its effect is profound. These patients lose all sense of hunger and must sometimes remind themselves to eat, or they will forget. When they do eat, they get satisfied very quickly and stop eating.
On average, patients lose 60 – 70% of their excess weight in the first year, and if they maintain the right habits, will keep that weight off. Diabetes resolution is very high and other weight-related conditions resolve with weight loss.
Some motivation is required as patients need to eat and drink properly, even without the sense of hunger or other motivations to do so. Acid reflux can worsen, so doctors are careful in their selection of patients who may have this procedure.
Gastric Bypass:
Gastric bypass remains the gold standard in modern weight loss surgery. It comes in many forms, but the Roux-en-Y is, by far, the most common and well-studied.
In this operation, the surgeon cuts the stomach, completely dividing it, forming in into a one-ounce pouch. The small bowel is divided, and one portion, the roux limb, is brought up and connected to this pouch. This means that food bypasses the remainder of the stomach and the first portion of the small bowel. The other part of the small intestine is connected to the roux limb, forming a “Y.” This allows the digestive juices from the stomach, liver, and pancreas to meet up with the food and digest it.
The result is significant weight loss. These patients lose an average of 75% of their excess weight in the first year. Acid reflux is cured immediately. Diabetes resolution is around 90% and all other weight-related conditions resolve as weight is lost.
The surgery, like the others, is done laparoscopically. Pain is minimal and goes away quickly. The hospital stay is one day, and patients may return to normal activities and work, as soon as possible – usually within a week or two.